WHG Helps Clients Understand and Navigate the Convoluted HCPCS Coding Pathways and Application Processes
- WHG is a member of the HCPCS Coding Reform Alliance. The Alliance is advocating for transparency, and separation of the coverage and coding process, among other problematic issues.
- Deb Wells has been recognized for her participation in the CMS HCPCS New Coding Application Beta testing and the HCPCS Coding Reform Alliance.
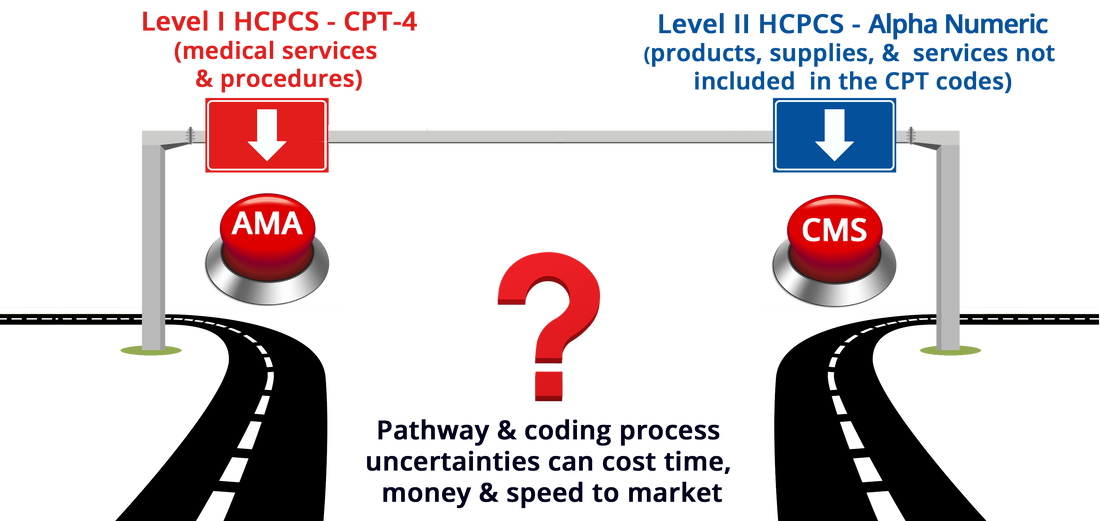
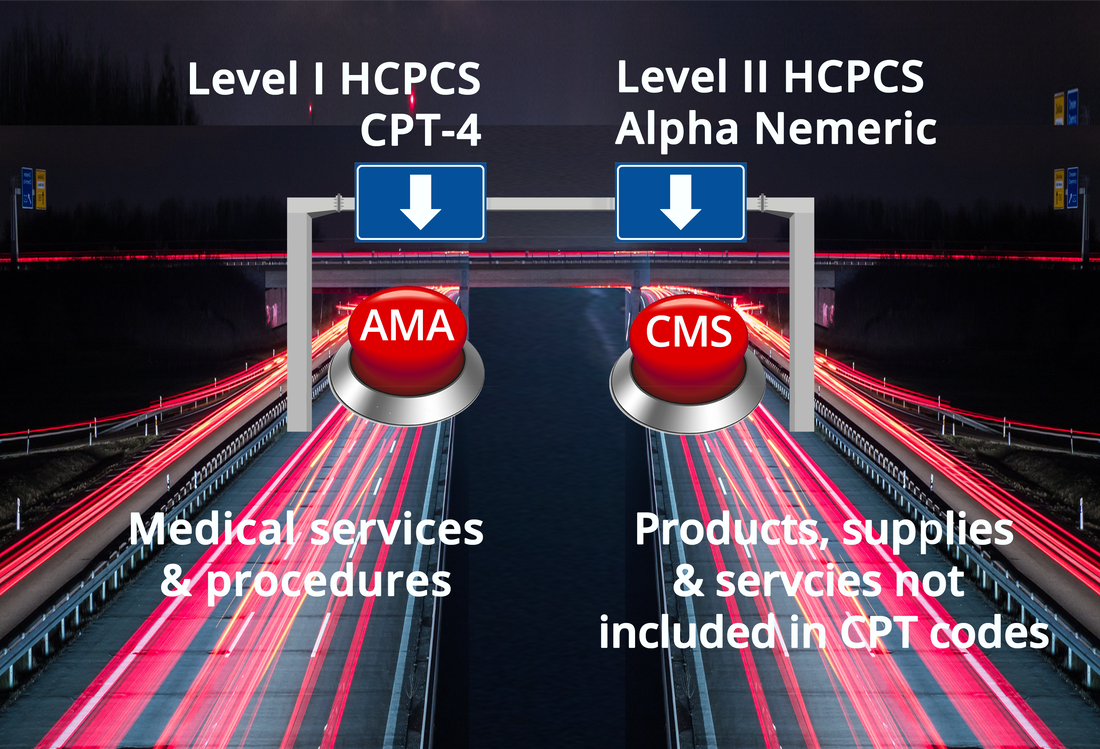
The Healthcare Common Procedure Coding System (HCPCS) is divided into two principal subsystems, referred to as Level I and Level II of the HCPCS.
- Level I - CPT-4 is maintained by the AMA
- Level II - Alpha Numeric is maintained by CMS
|
|
Our innovative approach to HCPCS Coding Consulting is Built on a Two-Step Sequential Process:
Critical to HCPCS Coding Success:
WHG's comprehensive reimbursement and market pathways are founded on 70+ years healthcare industry and government relations experience.
|
Each of the four (4) legislated Medicare insurance plans, (Part A, B, C, & D) covers different healthcare-related costs and pays for these well-defined services utilizing twenty (20) complicated fee-for-service and prospective payment systems.
Health Policy Challenges that Affect Reimbursement and Market Access
|
New FDA Emergency Use Authorization (EUA) regulations to allow for unapproved medical products or unapproved uses of approved medical products to be used in an emergency.
FDA approval and FDA clearance for non EUA medical products allows for commercialization. It does not mean that a product is covered or eligible for reimbursement by Medicare, Medicaid, or commercial insurance.
FDA approved indications for use and FDA product coding can result in downstream consequences with significant reimbursement pathway implications.
FDA controlled regulations affect CMS controlled policies determining site of care utilization, benefit category, coverage criteria and payment mechanisms.
Establishing new IPPS/HCPCS/CPT codes does not equate to CMS coverage or adequate payment, these reimbursement steps are separate CMS processes.
|
FDA regulations and CMS reimbursement processes are not intuitive and can lead to uncertainties and market access complications
Critical WHG Strategy Analytics - Prior to Submitting HCPCS Applications
|
Comprehensive Medicare, Medicaid and commercial insurance reimbursement pathway analysis.
Guidance through all 7-reimbursement steps - from diagnosis, treatment plan, site of care, and benefit category to coding, coverage and payment.
|
|
CMS utilization, mean costs and crosswalk data analytics are fundamental metrics of HHS and CMS decision-making trends.
CPT-RVU build up analysis - primary foundation of the annual Medicare Physicians Fee Schedule (MPFS) Rule Making process.
WHG categorizes the foundation of the hurdles identified in the 7-step reimbursement analysis and CMS analytics - executable milestones.
|
WHG identifies the current political and policy landscape
- Who can influence the change?
- What is the appetite for change?
Strategy analytics is the foundation for developing reimbursement pathways
WHG Focused Reimbursement Pathways
|
We identify the foundation of reimbursement hurdles or opportunities and prioritize executable milestones to maximize reimbursement:
|
We determine the pathway tactics once the actionable reimbursement strategies are defined and prioritized:
- Determine HHS and CMS policy jurisdiction
- Outline HHS and CMS decision-making processes
- Identify HHS and CMS key decision-makers and influencers
- Determine Capitol Hill policy jurisdiction, appropriations and oversight responsibilities
- Identify Capitol Hill key decision-makers and influencer
Are you Prepared for value-based payments? In the absence of evidence lower cost pressures will always prevail